Research Benno Hendriks
It’s important during cancer operations that the tumour is completely removed. In order to do this as accurately as possible, surgeons base their operation plan on images that were made during the diagnostic phase with imaging techniques. Surgeons then have to largely rely on their senses during the operation. According to Benno Hendriks, part-time professor of optics for minimally invasive instruments at TU Delft and research fellow at Philips Research in Eindhoven, we can do better. All too often, a piece of affected tissue is left behind or healthy tissue is damaged by the operation. This can lead to repeat surgery, extra treatments and worse patient outcomes. More feedback during the operation could change that. How? According to Hendriks by adding optical feedback in surgical instruments.
Put simply, it involves recognising tissue with the aid of light. Different molecules absorb and emit light at different wavelengths. We see that as colour, which is why blood is red, for example, and fatty tissue yellow. ‘With spectroscopy we look at these colours of the light. It enables us to distinguish more accurately than we can with our eyes,’ says Hendriks.
Biopsy needles made from optical fibre technology
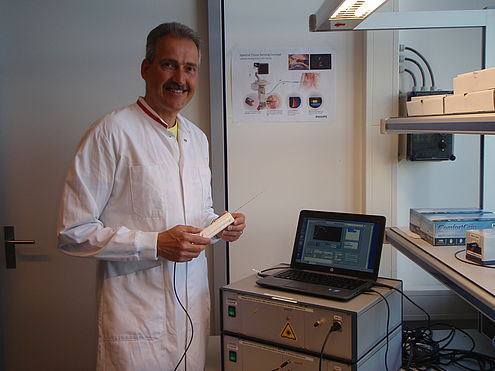
He applied that principle in recent years by providing biopsy needles with optical feedback. ‘When you take a tissue sample from a lung, for example, it inevitably moves during the procedure as a result of breathing,’ Hendriks explains. ‘So no matter how precise your X-ray or MRI images are, there’s always the risk of imprecision during the placement of the needle.’ To solve that dilemma, Hendriks and his colleagues equipped biopsy needles with optical fibre technology. ‘The ends of the optical fibre are placed in the tip of the needle. One optical fibre functions as a light source, which it shines into the tissue; another optical fibre collects the light that went through the tissue and that signal is transmitted to a detector,’ he explains. This makes it possible to read the tissue and determine whether it’s normal or abnormal tissue.
Of course, it has to first be clear how to distinguish between normal and abnormal tissue. A great deal of research went into that. ‘I measured all kinds of tissues in different situations in hospitals,’ Hendriks says. ‘To begin with at the pathology department with tissues taken from patients.’ He worked together with the Netherlands Cancer Institute for this, for example. Armed with knowledge about the tissue, he subsequently began to incorporate the technology into the biopsy needles. ‘That’s quite complex, because it’s a moving system. The last step in the development process is to then validate your instrument in practice.’
Introduction into the market
Once all these steps in the development process have been taken it’s up to the business unit – of Philips or another company – to assess whether it’s the right time to introduce the innovation into the market. Money plays a role of course. Hendriks also conducted research on the possibilities of using a similar system for nerve tissue recognition during local anaesthesia, for example. ‘During local anaesthesia you have to place the needle very close to the nerve. If you’re too far away from it, it won’t work. If you do it in the wrong place, you can damage the nerve,’ he says. Spectroscopic imaging of the nerve tissue would help. ‘But anaesthesia needles are quite inexpensive tools. There is always a limit to what the technology is allowed to cost. If an anaesthesia needle or a biopsy needle becomes too expensive as a result of the innovation, then it won’t be used after all.’
Smart surgical knife
Though it may seem as if new technology equates additional costs, in reality it can save a great deal in medical and social costs. Another of Hendriks’ ideas is to adapt the popular electric surgical knife, which is used to cauterise tissue. ‘You could make a knife like that smart, so that the tip of the knife recognises the tissue before you start cutting,’ he explains. ‘So it only cuts when you press on the button, and that can easily be integrated into the feedback loop. If it gives you a signal telling you to stop, then the knife stops immediately.’ However, you cannot take the spectroscopic tissue recognition that’s used in biopsy needles, for example, and use it in exactly the same way in a surgical knife. ‘This is much more complex, because when you cut, you also alter the tissue a bit in the vicinity of the knife. It’s similar to meat that turns brown when you fry it. In other words, it affects the optical signals that you’re receiving.’
‘We therefore have to first conduct all kinds of research on the interaction of the knife with the tissue,’ he continues. Back to square one, in other words, and to the pathology lab. And that’s just the beginning, because how do you then integrate the feedback into the knife with precision and simultaneously retain the other functions? Surgeons have to be involved in this research too. ‘How exactly do you use the knife? When is it useful for a surgeon to receive feedback? And then there are many other questions that will need answering in the coming years,’ Hendriks says. The surgical knife is only one example. ‘Many other instruments are used during operations, such as sutures and devices to make connections between intestines. You could make all of these smarter and thus prevent all kinds of complications.’
Innovation & cooperation
Integration and cooperation are indispensable factors in this. ‘The magic word for innovation in the medical world is “simple”. It has to be easy to use and intuitive,’ Hendriks says. ‘That’s also the approach at Philips: if you take your innovations to a hospital, make sure that they aren’t a bunch of loose components but a total concept.’ According to Hendriks it’s the concerted effort of all parties that determines an innovation’s success. ‘Part of the solution lies with companies such as Philips, part with TU Delft and another part with the hospital. So you have to start working together early in the process.’
He believes a good example is the coronary catheterisation lab, where diagnoses are made but also where stents are used to treat narrow arteries and heart valves are even replaced through the groin. ‘Something that used to require an open heart operation can now be done with an intervention that takes a couple of minutes. Once you’re done on the table, you can go home, so to speak,’ says Hendriks. ‘That’s the power of the integration of systems such as imaging, navigation and instruments. As a result, something highly complex has been made simple.’
Personal motivation
With his new chair, many of the components that need to be integrated in the operating room are coming together. ‘TU Delft, for example, is strong in building steerable instruments, such as those used in keyhole surgery. Here we are also looking at the workflow in operating rooms and how to train physicians to use new systems.’ Hendriks sees great opportunities ahead. ‘In most operations today, it all comes down to the skill of the surgeon. If you can manage to take image guidance from the diagnostic stage to the operating room, then you’ve already taken a big step forward. And if you can combine that with sensing technology and feedback, you’ll advance the entire field. That’s my goal.’
‘As a research fellow at Philips I have the opportunity to explore new directions and delve into my subject more extensively,’ Hendriks says. ‘Research at a company does have a different focus: a company opts for things that have potential today. A university has the liberty to look at things in the long term.’ He sees his dual role as an opportunity to bring the two closer together. ‘You can’t do it on your own. As a company, you can’t test all of the new directions that will become interesting in a few years. On the other hand, it’s of little use for a university to invest in potential solutions just to discover years later that no one wants to use it in practice. I want to help to bridge these two situations.’