Electrical implants
Small devices with huge potential
Since the introduction of the pacemaker in 1958, much has changed in the world of electrical stimulation. Whereas the first electrical implants targeted muscles, the implants of today are flexible and focus mainly on the nerves in our body. The concept, however, remains unchanged: electrical implants give control back to the body. Vasiliki Giagka, Assistant Professor of Bioelectronics at TU Delft, talks about the past, present and future of her field of research.
 Electrical implants of today look nothing like the first pacemaker of sixty years ago. They are much smaller now and have a much longer battery life, while being much more versatile. Small active implants now help us to relieve the symptoms of Parkinson’s disease, alleviate pain in different parts of the body and treat incontinence. According to Vasiliki Giagka, personalised electronics will soon be part of the treatment plan of patients with rheumatoid arthritis, asthma and diabetes, and patients with spinal cord injury will be able to walk again in the foreseeable future. A pipe dream? Giagka: ‘There is huge potential. I am sure there are a lot of people who will benefit from this research.’
Electrical implants of today look nothing like the first pacemaker of sixty years ago. They are much smaller now and have a much longer battery life, while being much more versatile. Small active implants now help us to relieve the symptoms of Parkinson’s disease, alleviate pain in different parts of the body and treat incontinence. According to Vasiliki Giagka, personalised electronics will soon be part of the treatment plan of patients with rheumatoid arthritis, asthma and diabetes, and patients with spinal cord injury will be able to walk again in the foreseeable future. A pipe dream? Giagka: ‘There is huge potential. I am sure there are a lot of people who will benefit from this research.’
Signals
Electronic implants can be used to control three modalities in the body: to induce signals that are interrupted, to record signals coming from elsewhere in the body to feed them back to another system and to block unwanted signals. ‘Consider how our bladder works,’ explains Giagka. ‘It fills up, so we have to empty it. There needs to be a signal that instructs our body to do this. This is a signal we can induce with electronics at a time we want to. But then we want to know precisely when we want to induce this signal. So we need to record information that reveals how full our bladder is. We can then use this information to extract a signal that tells us that our bladder is full and needs to be emptied. Some people suffer from urinary incontinence: their bladder empties without them having instructed it to do so. We can use electronics to block that signal and restore the mechanism. This way we close the loop.’
Weak points
Closing such a loop with electrical stimulation can heal patients with a variety of conditions, such as spinal cord injury. Giagka: ‘Here in Delft, we are doing research into electronics that stimulate the spinal cord to restore locomotion in paraplegic patients. They can then learn to walk again in a more coordinated way.’ Giagka was already working on this line of research when she completed her PhD in England. ‘I fabricated a flexible electrical implant to stimulate the spinal cord. I wanted to avoid using wires to and from the electronics, because they cause inflammation around the spinal cord. We are currently working on minimising the size and power consumption.’
About Vasiliki
 Dr Vasiliki (Vasso) Giagka (Athens, 1984) studied Electronic and Computer Engineering at the Aristotle University in Thessaloniki, the second largest city in Greece. After graduating in 2009, she moved to London to do her PhD at University College at the Analogue and Biomedical Electronics and the Implantable Devices Groups . She participated as a post-doctoral researcher in the GlaxoSmithKline Bioelectronics Innovation Challenge. Since 2015, Giagka has been working at TU Delft as an Assistant Professor at the Bioelectronics Group, where she carries out research into new materials and approaches to the problems that come with bioelectronic medicines. She also teaches Master’s students.
Dr Vasiliki (Vasso) Giagka (Athens, 1984) studied Electronic and Computer Engineering at the Aristotle University in Thessaloniki, the second largest city in Greece. After graduating in 2009, she moved to London to do her PhD at University College at the Analogue and Biomedical Electronics and the Implantable Devices Groups . She participated as a post-doctoral researcher in the GlaxoSmithKline Bioelectronics Innovation Challenge. Since 2015, Giagka has been working at TU Delft as an Assistant Professor at the Bioelectronics Group, where she carries out research into new materials and approaches to the problems that come with bioelectronic medicines. She also teaches Master’s students.
Local treatment
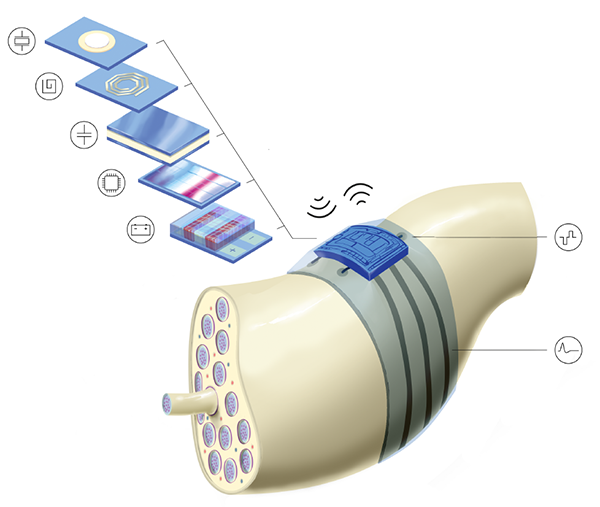
Giagka’s current activities focus on the next generation of active implantable devices: Bioelectronic Medicines. ‘They are even smaller than the current options and target the peripheral nervous system: smaller nerves that transmit signals of sensation and motor function through the whole body. A doctor must be able to inject the tiny implant around a nerve through a needle and program the device to give the patient personalised local treatment. That has a big advantage: only the immediate vicinity is treated, which avoids the possible side effects that come with medicine.’
Challenges
Giagka believes that before we are at a stage when a doctor can inject and program such an implant, we still face a number of challenges. ‘The devices must be biocompatible with the body and the anatomy, so that they do not cause any damage. They also need to last for decades and be able to run and communicate wirelessly.’ It is not yet known what these active implants will look like. ‘We want to concentrate all the technology in a small housing with a three-dimensional cuff-like form, which can be placed around the nerve. It would be really great if we could make an implant the size of one cubic centimetre.’ Since pharmaceutical company GlaxoSmithKline organised a competition to develop a wireless active implant a few years ago, many companies are now investing in the market. ‘Active implants have since become a hot topic,’ says Giagka. ‘I cannot say whether it is feasible, but GlaxoSmithKline hopes to be able to market these implants by 2023.’