Biomechanical Engineering’s fiftieth anniversary
The Department of Biomechanical Engineering will be celebrating its fiftieth anniversary in 2018. It’s still a relatively young department in a faculty that’s more than 150 years old, but nonetheless this is a moment well worth celebrating. How were the foundations of Biomechanical Engineering laid, one of the Mechanical, Maritime and Materials Engineering (3mE) faculty’s seven departments at TU Delft? In order to highlight this anniversary, this story recounts some anecdotes from the past fifty years.
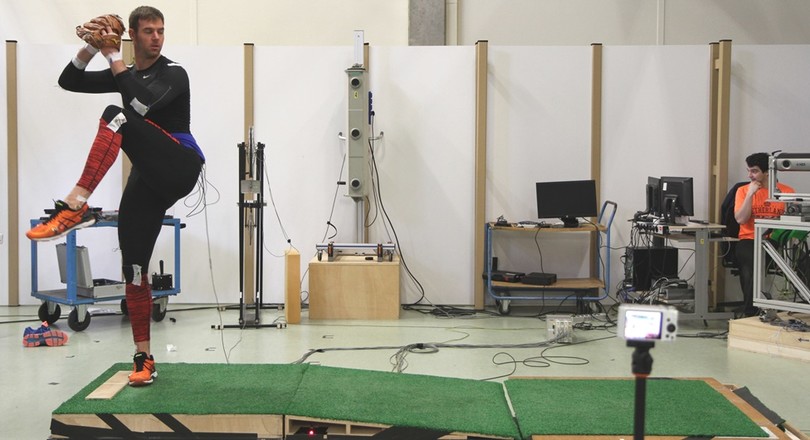
Physical performance is crucial to athletes and people with physical restrictions. A doctor thinks and takes action based on the medical problem at hand. The engineer and scientist approaches the problem from a technical point of view and attempts to gain a fundamental understanding of it, after which he or she will look for a technical solution. When they converge, special things happen. From an insulin injection system for blind diabetics to a model of the blood flow through the heart, and from a measuring bike to a measuring ice skate for amateur and professional athletes alike, and a feedback system for pitching mechanics in baseball.
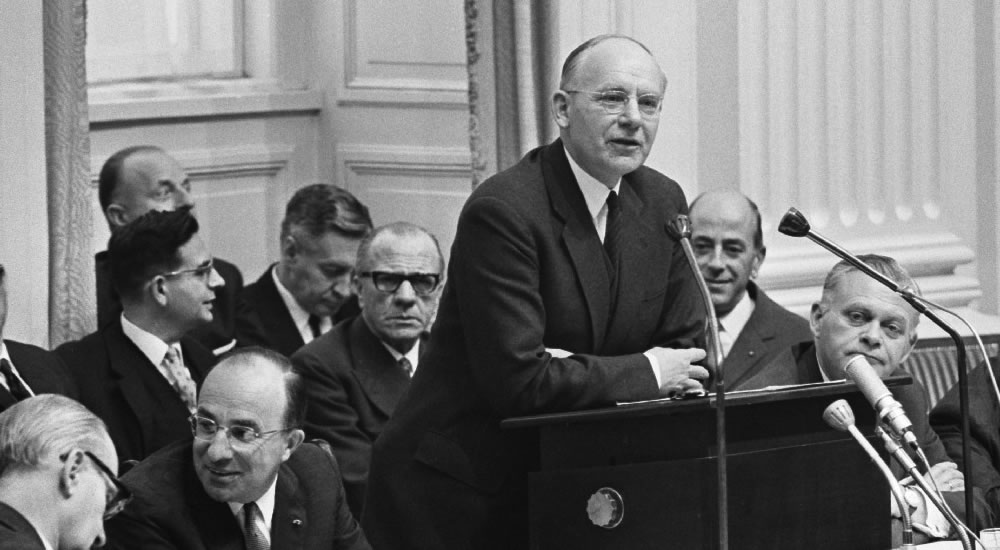
 As a ‘ceremonial date’ for Biomechanical Engineering’s fiftieth anniversary, we have chosen the PhD ceremony in December 1967 of Henk Stassen, an out-of-the-box thinker who was one of the first to introduce innovative engineering techniques into the medical profession.
As a ‘ceremonial date’ for Biomechanical Engineering’s fiftieth anniversary, we have chosen the PhD ceremony in December 1967 of Henk Stassen, an out-of-the-box thinker who was one of the first to introduce innovative engineering techniques into the medical profession.
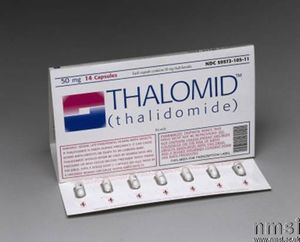
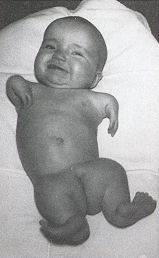
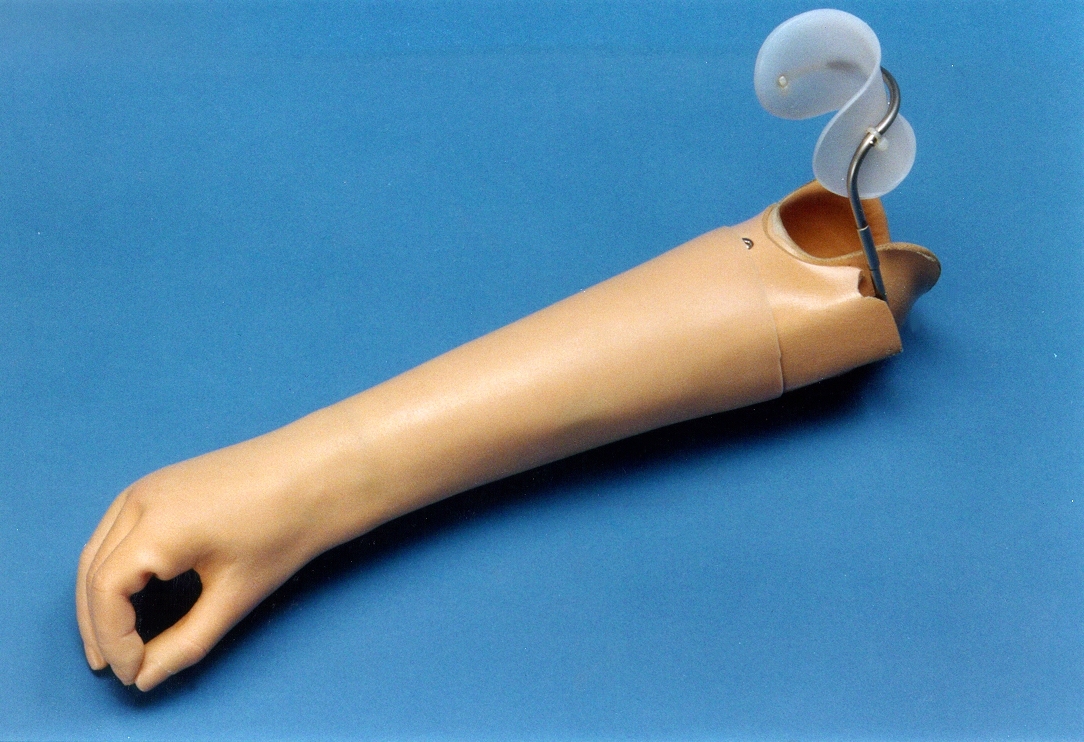
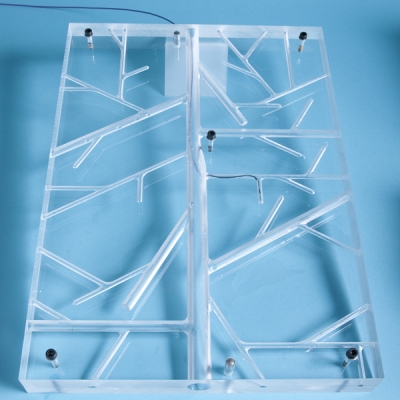
A defining moment in the genesis of the Department of Biomechanical Engineering was the introduction of Thalidomide in the market. Thalidomide was the active substance in what was generally known as ‘Softenon’ in the Netherlands, a drug used to fight nausea and insomnia in pregnant women. This medicine turned out to cause birth defects: children were born with deformities in their arms and legs. In the Netherlands, 25 ‘Softenon children’ were treated in the Maartenskliniek in Nijmegen with so-called ‘Heidelberg Prostheses’ – poorly functioning, pneumatically driven prostheses that were unreliable and had gas canisters with CO2 that ran out too quickly. A doctor from Nijmegen approached professor Boiten, head of the Department of Measurement and Control within the Faculty of Mechanical Engineering. ‘You guys in Delft know a lot about measurement and control technology and about pneumatics, please help us,’ the doctor asked the professor. Boiten set two working groups to the task: ‘instruments’ and ‘human-machine interaction’. This is how mechanical engineers at Delft became involved in prostheses and how initial contact with the medical world was established.
In 1967 the Orthoses Prostheses (the WOP) working group was set up, a partnership between De Hoogstraat rehabilitation centre in Leersum, TU Delft and TNO’s Institute of Medical Physics. Here, the intensity, development and scope of the work being done for Softenon patients was given a boost, and the different parties joined forces to help people with a physical restriction in a multidisciplinary way. That is still happening, but now under the name Biomechatronics & Human-Machine Control.
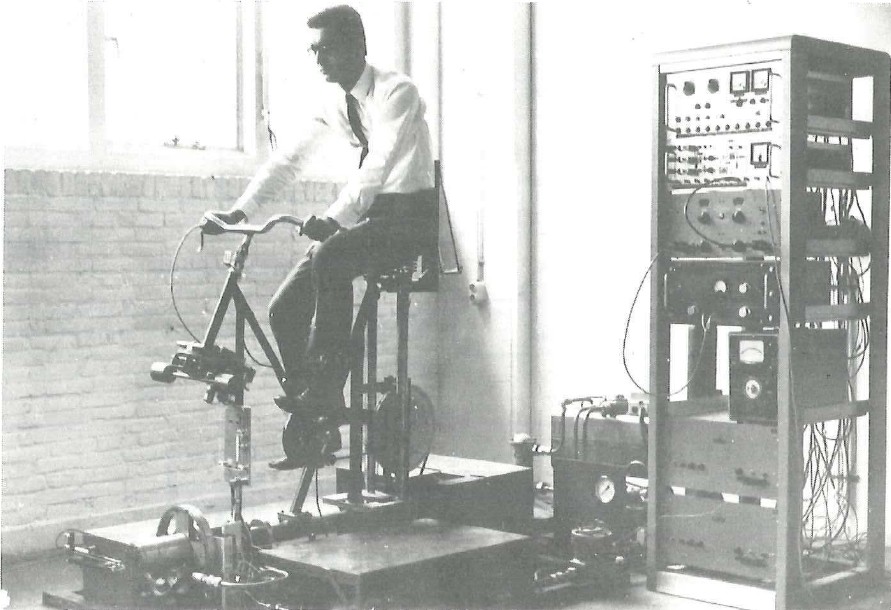
Carried out in parallel with the research on orthoses and prostheses was a slightly more frivolous line of research, also medically oriented. Research was being conducted by the measurement and control and human-machine systems groups on how use of alcohol and mind-altering substances affects cycling behaviour and the stability of the bicycle and cyclist. These kinds of things were possible in those days. In collaboration with the Jelgersma clinic in Leiden, vodka was served to test persons on bicycles in the lab. Later, the same group took the first steps towards developing a light-spot operated typewriter for disabled people. The interaction with the medical world has remained a source of inspiration.
And so ‘bio’ and ‘mechanical engineering’ continued to grow closer together.
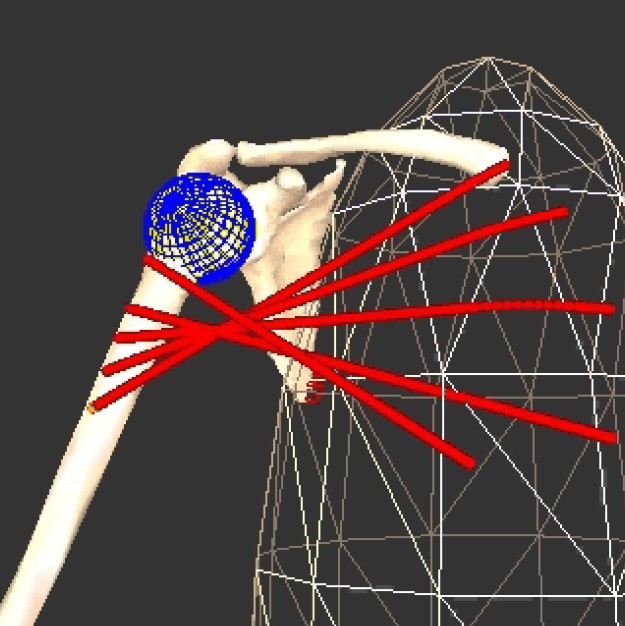
Through his clinical contacts, Henk Stassen was exposed to clinical problems concerning injuries to the brachial plexus, a network of nerves approximately at the height of the collarbone that ‘guide’ the arms. Brachial plexus injuries often cause the arm to cease functioning properly, though the hand continues to function. Convinced that treatment could be improved, he set up a project to develop an expert system for the early prediction of the loss of function following an accident and develop a biomechanical model that would make it possible to predict the required operations. This first model became the Delft Shoulder and Elbow model, which is used worldwide and still serves as an inspiration for new models of both the upper and lower limbs.
Research faced a familiar problem back then as it does today: how do you finance the research and where do you get the people from? In the 1970s, conscientious objectors provided a solution: you could get them for a reasonable price through the Ministry of Social Affairs. Henk Stassen had met Anne Vondeling, former minister of finance and a prominent member of the Dutch Labour Party, at the rehabilitation centre in Leersum. Anne Vondeling was recovering there from a serious car accident. He advocated using a large number of conscientious objectors who could start working in the Human-machine Systems and Instruments working groups instead of serving in the army. Many of these ‘unconscionables’, as they were referred to, never left the department again.

 The bicycle research continued, but without the alcohol and medicine. Now the research was no longer medically oriented but based on human-machine interaction. Just like the ‘supervisory control’ research that began in the mid-1970s. People launched satellites from control rooms or monitored major nuclear installations. What’s a smart way of setting up a control room, and how do you ensure that people respond adequately to warning signals? This research laid the foundation for the later development of DORA, the Digital Operating Room Assistant. From aerospace to the operating theatre and back again: the research on prostheses and orthoses was the point of departure for ‘manual control’ projects, such as the development, with the European Space Agency, of remote-controlled robot arms in space station.
The bicycle research continued, but without the alcohol and medicine. Now the research was no longer medically oriented but based on human-machine interaction. Just like the ‘supervisory control’ research that began in the mid-1970s. People launched satellites from control rooms or monitored major nuclear installations. What’s a smart way of setting up a control room, and how do you ensure that people respond adequately to warning signals? This research laid the foundation for the later development of DORA, the Digital Operating Room Assistant. From aerospace to the operating theatre and back again: the research on prostheses and orthoses was the point of departure for ‘manual control’ projects, such as the development, with the European Space Agency, of remote-controlled robot arms in space station.
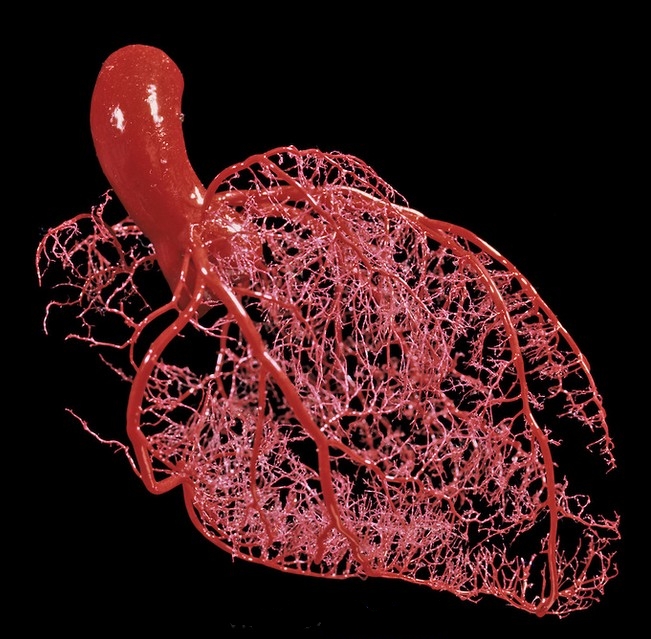
In the late 1970s, a new project was set up: modelling the blood flow through the heart muscle from the perspective of measurement and control. The model was based purely on mechanical engineering mathematics, which also used measurements taken during heart surgery. This knowledge and experience led to the first developments in minimally invasive surgery.
In both cases, the approach to the modelling of the heart muscle and the involvement with surgery was unique from a technological point of view and led to innovative results. In around 1997, a major grant was secured in the shape of the DIOC9 programme (the Delft Interfaculty Research Centre). Researchers used this incentive to allow the MISIT lab (Minimally Invasive Surgery and Interventional Techniques) to fully flourish. The researchers liked to let nature inspire them when thinking about new techniques and designing new tools: the chameleon’s retractable tongue, the sting of a wasp and the agile arm of the octopus.
In addition to shoulders, arms and hands, the focus in the 1990s was also on legs. A two-legged walking robot took its first steps at the Department of Biomechanical Engineering. A student was allowed to design the robot legs on the condition that they were not electronically driven. The student succeeded, by having the legs walk from a slight incline. Our knowledge of the human body was used to let a robot walk. Our knowledge of robot legs, in turn, was used to allow people with physical restrictions to walk with the aid of exoskeletons and other kinds of technical walking aids. The knowledge that was being built up in all of these different disciplines in the department gradually evolved into a large (bio)robotics section. Recently this robotics section was brought together with other lines of research in the area of robotics in the 3mE faculty in a new Department of Cognitive Robotics.
The Biomaterials line of research was once part of Materials Engineering at TU Delft. This line of research no longer dovetailed with the direction that Materials Engineering was going in, but all the more so with that of Biomechanical Engineering. The adoption was handled swiftly. In 2011 the Biomaterials group joined the Department of Biomechanical Engineering. Biomaterials are extremely important for the development of both medical tools and prostheses and implants. The potential of 3D-printing adds new dimensions to this research. By developing biomaterials with special properties, which can unfold, contract or bend by means of specific triggers, for example, researchers are able to work on smart implants for the future.
Many years of research provided a solid foundation to launch the master programme in BioMedical Engineering in 2004. This was an initiative of Biomechanical Engineering, in collaboration with Electrical Engineering, Applied Physics and Mechanical Engineering. Many employees, lecturers and researchers at Biomechanical Engineering were also involved at the inception of the Clinical Technology bachelor programme in 2014 and the Technical Medicine master programme in 2017, a partnership between TU Delft, Leiden University Medical Center (LUMC) and Erasmus University Rotterdam (Erasmus MC). You could see this as the culmination of many years of productive cross-over collaboration between technical and medical science.
As incomplete as this story may be, it shows how Biomechanical Engineering evolved into a multi-faceted and flourishing department by delving deep into the material and simultaneously remaining open to questions from the outside, collaborating with other departments, listening to patients, athletes and medical professionals and, in the spirit of the founding father Henk Stassen, continuously embarking on new paths.