Freedom in a Frame
Promotores: Jop Groeneweg
PhD: Nienke Luijcks
In collaboration with: UMCG (Maarten van der Laan) Amsterdam UMC (Annelies Visser, Dave Dongelmans)
Planned period: June 2021 - July 2022
Project summary: The number of procedures and guidelines in healthcare can negatively affect professionals. By emphasising their needs, they experience more autonomy and enables them to use their skills and knowledge better. This will also improve the work process.
About the project
With the Freedom in a Frame approach, we redesign complex work processes to fit healthcare professionals’ needs. We look at similarities and differences in the system world (Work-as-Imagined) and the living world (Work-as-Done) to gain better understanding of how professionals interact in their work. Here, we will have a closer look at the procedure that was researched in the study.
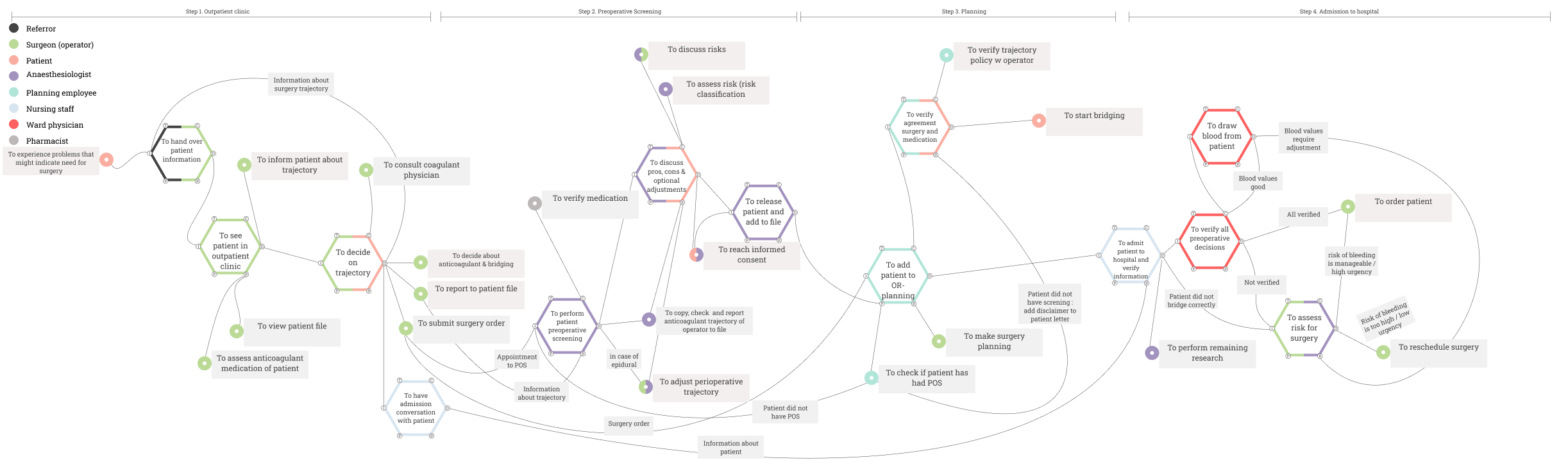
We studied the perioperative trajectory with a focus on anticoagulant medication in two academic hospitals. Specifically, the perioperative trajectory is the period before the patient is admitted for surgery. For Work-as-Imagined, we studied the protocols related to the trajectory. For Work-as-Done, we conducted qualitative interviews with healthcare professionals in different roles who are involved in the perioperative trajectory. Finally, these findings were visualised using the functional resonance analysis method (FRAM).
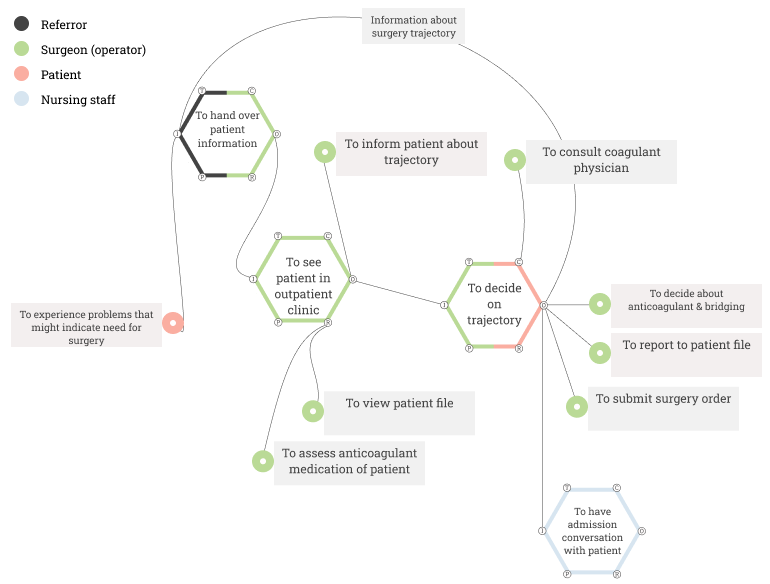
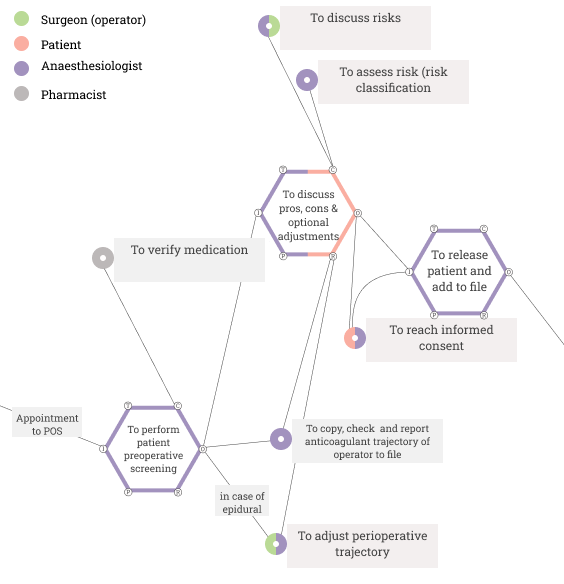
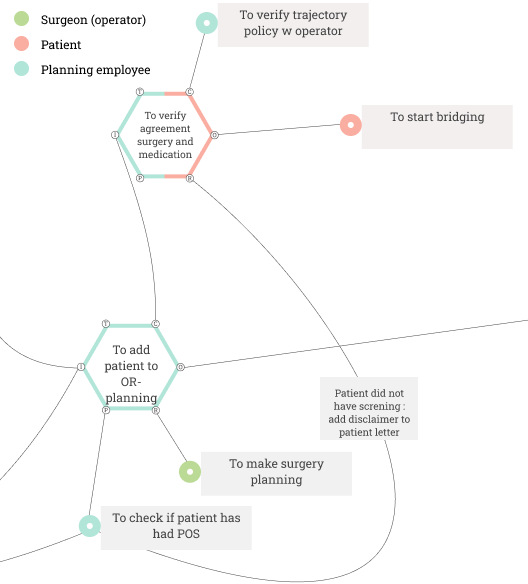
In this overview, we will go through the Work-as-Done of one of the two hospitals. We focused on the first part of the perioperative trajectory. The trajectory can be divided into four steps:
- Outpatient clinic
- Pre-operatory anesthesiological examination
- Planning
- Patient admission
This project is presented as a research poster during BMJ International Forum 2023 in Copenhagen. The poster can be viewed on the right.
In step 1, the general practitioner, the patient and the surgeon are involved.
During the first step of the perioperative trajectory, the surgeon and the patient are actively involved. The surgeon receives an information letter stating that surgery might be necessary from the patient’s general practitioner. In addition, the surgeon might already possess information about the patient in the electronic health record. The patient visits the surgeon during the outpatient clinic. During this visit, the surgeon assesses whether surgery is necessary by talking to the patient and looking at their file. In addition, the patient is asked what anticoagulant medication they use.
Then patient and surgeon come to a consensus about the patient’s trajectory. In complex cases, a healthcare professional specialising in anticoagulant medication can be consulted. Based on this consensus, informed consent is given by the patient. The decision about the trajectory is communicated back to the general practitioner. The information from this visit is written down in the electronic patient record, and a surgery order is submitted by the surgeon. The surgery order leads to an appointment for the patient with the anesthesiologist. It is possible that the nursing staff already has the admission conversation with the patient, otherwise, this will happen in step 4.
In step 2, the anesthesiologist, the pharmacology assistant, the patient, and (in some cases) the surgeon are involved.
With information from the electronic health record, the anesthesiologist meets the patient for the pre-operatory anaesthetic screening. During this screening, the pharmacology assistant verifies the patients’ medication, this also concerns anticoagulants. In addition, the anesthesiologist discusses the pros, cons and possible risks of the procedure with the patient. If necessary, the risks can then be discussed by the surgeon and anesthesiologist together.
If the patient will be given an epidural during surgery, the patient’s trajectory as written by the surgeon might have to be adjusted. At the end of the screening, both patient and anesthesiologist reach informed consent about the anaesthesia for surgery. Afterwards, the patient is “released” by the anesthesiologist and the required information is added to the electronic health record.
In step 3, the planner, the patient and the surgeon are involved.
The surgery order submitted by the surgeon leads to the planner adding the patient to the OR planning, but before doing so the planner has to check whether the patient has had the pre-operative screening and has been released by the anesthesiologist. In addition, the surgery planning that is made by one of the surgeons is required for the planner to add the patient. If the patient did not have the screening, a disclaimer is added to the letter that is sent to the patient before surgery. In addition, the agreements about the surgery and medication are verified by the planner with the patient. The planner also verifies the trajectory with the operator. If this is all finished, the patient can start bridging.
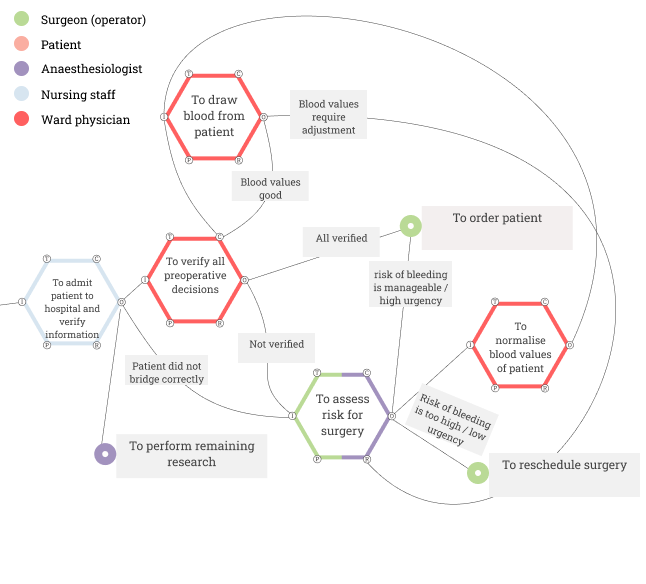
In step 4, the nursing staff, the ward physician, the patient, the anesthesiologist and the surgeon are involved.
A day before surgery, the patient is admitted to the hospital. The nursing staff then admits the patient and verifies their information. If necessary, the anesthesiologist can still perform some remaining research. In addition, the ward physician verifies the preoperative decisions and they draw blood from the patient. Either the nursing staff or the ward physician can signal whether the patient adjusted their anticoagulant medication correctly. If the blood values of the patient are good and they adjusted their medication correctly, the patient can be ordered for surgery. If this is not the case, the surgeon and anesthesiologist assess the patient’s risk for surgery. If the risk of bleeding is manageable and there is a high urgency for the patient, the patient can be ordered for surgery. If the risk of bleeding during surgery is too high and the urgency is low, they can decide to reschedule the surgery.
Altogether, these four images combined lead to the Work-as-Done that was researched in this study, the full overview can be seen below. This visualisation of the work process in practice was then compared to a similar visualisation of the Work-as-Imagined. This comparison is named a gap analysis. Both the Work-as-Imagined and Work-as-Done were discussed in a focus group with healthcare professionals. Based on the findings during the focus groups, we designed micro-experiments. Micro-experiments are small adjustments to the work process in practice, to test whether this improves the effectiveness and efficiency of the process.
What is FRAM?
FRAM is a tool that is used to visualise work processes designed by Erik Hollnagel. This tool shows how different steps, or functions, in a process are interconnected. This can be in different ways. Functions can be connected through input (I), output (O), resource (R), precondition (P), time (T) or control (C). For instance, a function can be a precondition if it has to happen before another function can be done. You would have to plug in a coffee machine to make coffee, otherwise, the machine will not work. These six connections are the six corners of the hexagons that you can see in the following images.