In India, sterilisation has been the most common method of birth control since the 1970s. More than one in three women are being sterilised at the moment. A lot of these operations take place in what are sometimes dubious private clinics, where women undergo an open operation via a large incision, so it takes a long time for them to recover. Moreover, there is a serious risk of infection because the environment is often not sterile. Tim Horeman wants to make a change by developing affordable and innovative instrument for surgery.
Horeman: ‘I am developing instruments to perform these sterilisations with laparoscopy, otherwise known as minimally invasive surgery. The doctor makes a small incision in the belly, then inserts an instrument with a camera and places a clip around the oviduct.’ Operating like this means the doctor has to cut through less tissue, so women are mobile again within a few hours.

Minimally invasive surgery for low-resource settings
Recently, Horeman and his colleague Jenny Dankelman, professor of minimally invasive surgery and intervention techniques, were awarded a significant grant from NWO/ZonMw for their initiative. Their research focuses on the development of affordable and innovative instruments for minimally invasive surgery, to be used in hospitals in low-resource settings. Such as situations where a sterile operating room is not available. This would make the surgery cheaper, but also safer and easier to perform. In their initiative, Dankelman and Horeman are working together with Prashant Jha from the School of International Biodesign of AIIMS and IIT Delhi and his Indian partners from the Surgery Department and the Community Medicine Department of AIIMS Delhi in this research.
A more sustainable and accessible grasper
In his Minimally Invasive Surgery and Interventional Techniques Lab (MISIT), Horeman and his colleagues are developing a wide variety of instruments for minimally invasive surgery. ‘A lot of instruments are usually thrown out after a few operations.’ That is because they cannot be disassembled and so cannot be cleaned. Such as the gold standard for laparoscopic graspers (8 millimetres) currently on the market, which is operated by surgical robots. ‘This instrument is driven by four motors that can turn the instrument in two lateral directions and make them open and close,’ says Horeman, who took apart the instrument and counted 72 parts, including as pins, wheels, tubes, springs and cables. ‘On top of that, operation robots are being increasingly used: every year there are 55 additional robots in circulation. It may sound ambitious, but scientists expect 35 per cent of all laparoscopic operations to be performed by robots by 2025 (Forbes). If we are still using the same device technology by then, our landfills will be cluttered with 10 million used instruments a year.’
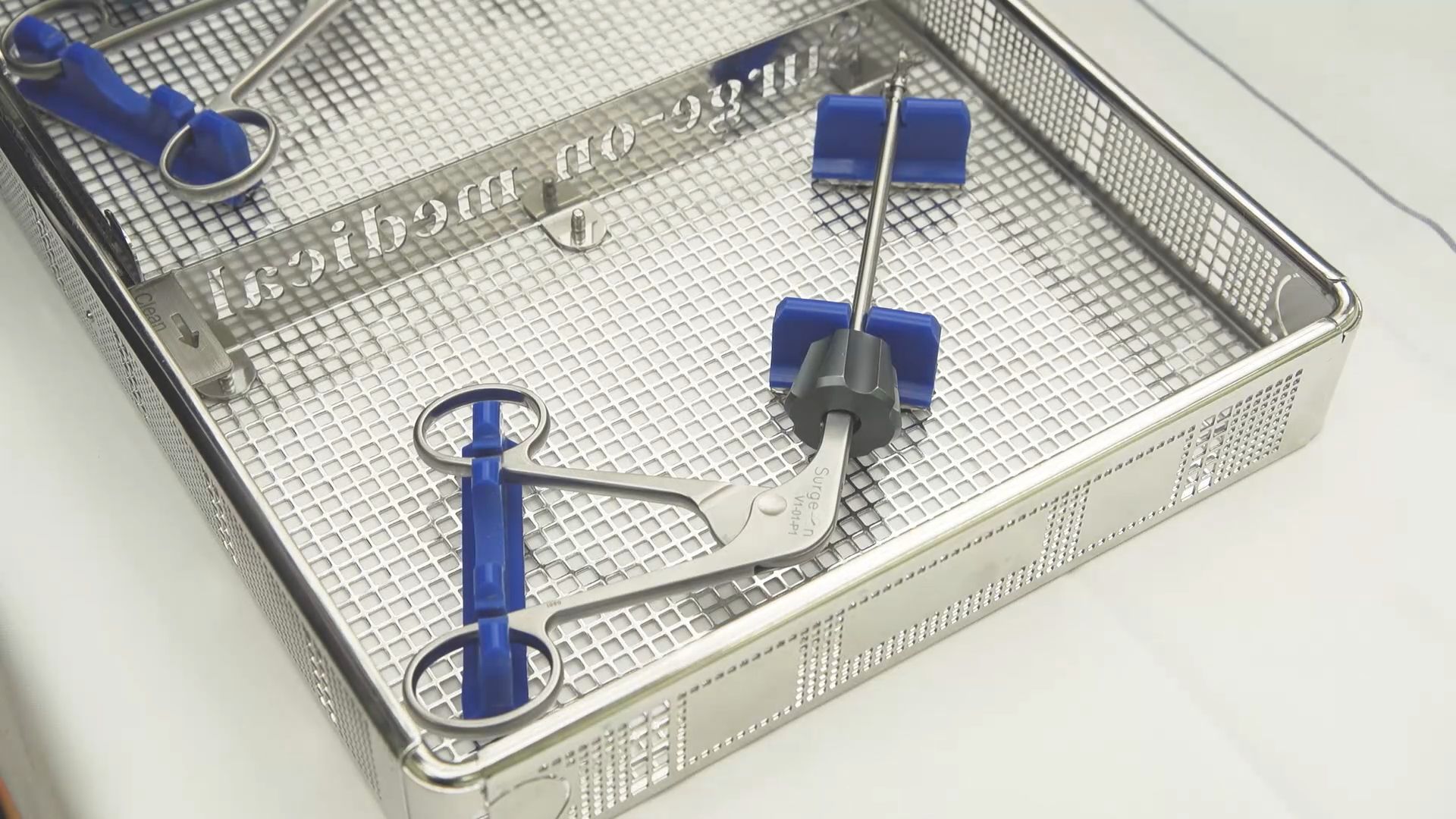
Horeman has come up with a more sustainable version of the standard grasper. ‘There are three layers of tubes in it. It is 5 millimetres thinner than the existing one and also contains 70 per cent fewer parts. You can completely take it apart so all that is left are the tubes and tip of the instrument, which you can open up and then clean using the standard sterilisation protocol in the hospital.’ The fact that the grasper can be reused generates huge savings for the hospital, which makes the minimally invasive operations affordable. ‘The instruments that you have to keep throwing away during robot surgery cost an additional 4,000 to 5,000 euros per procedure, on top of what laparoscopy already costs. So this new technique, which is now being further developed under license by the company Surge-On Medical, is not only making the medical world more sustainable, but also more accessible for surgeons.’
But that’s not the only advantage of the new grasper. Doctors can attach a grip that allows them to rotate the shafts with two wheels and a trigger. That’s not possible with the current designs of these instruments, because they always have to be operated by a surgical robot. Now that grasper can be used in areas for which there is no surgical robot.
Steel and electricity
According to the biomedical engineer, a major scientific challenge still lies ahead. He now wants to construct the steel components in the instrument in such a way that they can conduct electricity to close tissue. ‘When you operate, you often have to cut tissue in half. That causes bleeding. To stop the tissue from bleeding, you could put a clamp on it that has a current running through it. That would enable you to close the vessels by burning them,’ he says. To achieve that, Horeman is going to work with physicists who have knowledge about fusing/vaporising materials with different properties.
Horeman: ‘If we can manage to do that, then we will not only have made huge strides mechanically but also at component level. Then you are working on a new generation of instrument construction.’
A mini-clean operating room
Together with Dankelman and the company MediShield, Horeman has also come up with a solution for hospitals that lack operating rooms: the mini-clean room, a modular, dividable screen that shields the instruments and wound at all times from the environment and which can easily be moved and set up in rural areas in less developed countries.
And last but not least, Horeman envisions a future in which you no longer have to rely on experts to maintain the parts of a robot or instrument. ‘That is not compatible with sustainable surgery. I want people to be able to maintain, clean and assemble things themselves on-site. So you have to train them: technology is never the only solution.’
Global Research Areas
| Health | |
| Water | |
| Energy | |
| Disaster Resilience and Response | |
| Urbanisation |
Contact

Tim Horeman



