Clinical technologists increasingly trusted
The Bachelor's degree programme in Clinical Technology was launched six years ago. The aim of this new programme was to bridge the gap between medical experts and engineers. The prospects of clinical technologists on the job market are looking good. And rather than holding them back, the coronavirus pandemic now seems to be a driving force behind this process.
Collaboration between medicine and technology lies at the heart of the Clinical Technology programme. Clinical technologists look at the human body from an engineer’s perspective, working with the latest technologies in healthcare. This is a joint programme between TU Delft and the medical faculties at Erasmus University Rotterdam and Leiden University.
According to its Director of Studies, Pleun Hermsen, last year saw two crucial developments that will help boost the job market for clinical technologists. “Since recently, they have been able to join the BIG-register of recognised healthcare professions. This gives clinical technologists a protected professional title and the power to perform certain medical procedures. They are also now permitted to initiate their own treatment processes and claim the costs. This is making it an increasingly interesting position for clinical practice.”
In Hermsen's view, the coronavirus pandemic has accelerated crucial changes in healthcare: “I sense that there has been a kind of paradigm shift and clinical technologists could turn out to be even more important than they already were.”
Forging a link
So, what exactly does a clinical technologist do? Hermsen: “In healthcare, there are numerous unresolved medical problems where the embedding of technology can prove advantageous. A clinical technologist is someone who understands both the technology and the medical side and can help to find solutions by forging a link between the two domains.”
That link is needed to bridge the age-old gap between doctors and engineers. Hermsen has previously described doctors’ reluctant attitude towards clinical technologists as ‘cold feet’. The end of that phase now appears to be in sight, agrees Tim Boers, who chairs the Dutch Association for Technical Medicine (NVvTG). “This fast-growing professional group is quickly spreading across the healthcare landscape. As a result, our added value is being increasingly recognised.”
Sell yourself
Martine Breteler agrees. “I’ve noticed that, as a technical physician, you really have to sell yourself and show what you’re capable of – much more than a doctor needs to do.” Breteler is a technical physician at UMC Utrecht and conducts research into wireless monitoring of patients in nursing wards and at home just after being discharged from hospital. “We use sensors, wearables and smart algorithms to monitor patients’ vital functions in an attempt to prevent them falling into remission unnoticed.”
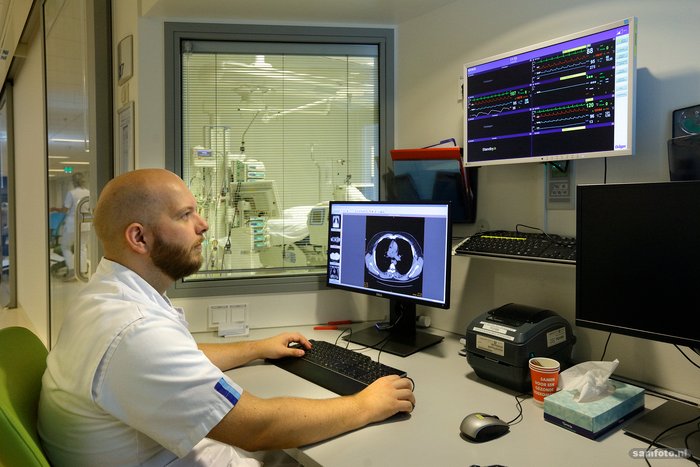
The outbreak of the pandemic gave Breteler a unique opportunity to demonstrate the added value of the profession: “Covid is a very unpredictable disease. Patients’ conditions can deteriorate suddenly when you least expect it. That’s why, on the Covid ward, I was immediately asked to implement continuous patient monitoring. We kept track of patients’ breathing, heart rate and oxygen levels from a control room. To take the pressure off the nurses, medical interns and students of technical medicine from the University of Twente were on hand to monitor trends, sounding the alarm if things started to go wrong.”
In just a few weeks, Breteler introduced a system that would normally take a year to prepare. “We worked incredibly hard and I also really noticed that my role as a technical physician was of huge added value, surpassing anything a doctor could have offered.”
Trust in the profession
Peter Somhorst already works as a technical physician in the Intensive Care (IC) department at Erasmus MC. “When I started, more than five years ago, I noticed the team were wondering why they should trust my knowledge of medical procedures. Since then, I’ve seen that trust in me and our profession has grown incredibly.”
Somhorst is working on electrical impedance tomography (EIT), a technology used to optimise patients’ breathing (including Covid patients) in consultation with the intensive care doctor. At the peak of the pandemic, his advice and respiratory expertise became increasingly important. “The demand for my expertise increased hugely and my advice was accepted much more easily than five years ago.”
Students are also noticing increasing acknowledgement of the profession of clinical technologist. Joris Behr, chair of the Clinical Technology Study Association (S.K.V.T) Variscopic: “When I started this degree, three years ago, doctors often asked me what I actually did. I now notice that there’s much more support and interest.” Behr mentions Operation Air, a project at the height of the Covid crisis in which fifty students proved that it’s possible to develop a new ventilator in the space of three weeks. The project received national and international acclaim.
Fleur Brouwer completed her Master’s in Technical Medicine on 10 July 2020, making her one of the first ten graduate clinical technologists in Delft. She has never had any concerns about her job prospects. “You get such a wide-ranging education. Because of that, I think it’s purely up to you to decide what you enjoy most.”
Job opportunities
According to the chair of the NVvTG Tim Boers, clinical technologists have never had a problem finding employment. Apart from a few positions in industry, these tend to be research jobs and PhD positions that doctors and biomedics could also apply for. “It was – and still is – difficult to start out in a clinical setting from the get go,” says Boers. “That’s now changing for the better, with increasing numbers of fellowships.” A fellowship is a clinical training programme in which a clinical technologist specialises in one or several medical disciplines.
This is also what Fleur Brouwer hopes to do. “Ideally, I would like to do a fellowship in the IC at Leiden University Medical Center, were I also did my graduation internship. I hope to hear soon whether that will go ahead.”
Martine Breteler and Peter Somhorst see the fellowships as a positive development. In our view, there should be more of them and the education of clinical technologists should go a step further. Somhorst: “A technical physician or clinical technologist has a very wide-ranging educational grounding. A fellowship is a great start to a career in clinical practice and a good first step towards clinical specialisation, but it would be nice if, as in the case of a junior doctor, there was a clear training pathway, quality standards and ultimately registration as a specialist. At the moment, that’s not yet the case.”
Covid
Opportunities within clinical practice do not necessarily need to take the form of a fellowship. Recently, the Internal Medicine and Diabetes Care department at the Radboud University Medical Center in Nijmegen opted to appoint a clinical technologist instead of an internist. “It was a deliberate choice”, explains internist and clinical pharmacologist Bas Schouwenberg. “Most of the care for diabetics is about self-management and it increasingly involves technology. Pumps, sensors, closed-loop systems ensuring that patients receive the right amount of insulin almost automatically, and various types of software. It’s all fantastic, but we want to be able to supervise it all more effectively. A clinical technologist can treat patients and also help us to enhance the quality of care.”
The fact that the Radboud vacancy has emerged now is no coincidence. Schouwenberg: “It’s been in the pipeline for a while. Covid has just emphasised why we need to make it happen.” Schouwenberg explains that there has been talk of an online video system for remote care for years. “It has never actually happened. It was seen as ‘not secure’ and we couldn’t claim on the insurance without a physical consultation. Things like that are now suddenly possible.”
‘The BIG-regiser gives them a protected professional title and the power to perform certain medical procedures’
Springboard
“That’s the paradigm shift I’m referring to,” says Pleun Hermsen. “A huge opening has emerged for remote care, offering opportunities and jobs for clinical technologists in clinical practice.” Tim Boers adds: “It’s difficult linking something positive to the pandemic, but it’s become a springboard for reaching greater heights more quickly.”
Pleun Hermsen puts this in a wider context: “There are still countless unsolved medical problems. These are situations in which you’d actually like a clinical technologist to have some input.” There are regular occasions when this does not happen because teams in the clinics are unaware of the possibilities. In that sense, Hermsen believes there is a latent need for clinical technologists.
Boers feels the same. He conducts research into the treatment of benign thyroid tumours. “Broadly speaking, you have two options: you either cut out half of the thyroid gland or insert a needle and burn away the tumour from inside. It’s a technique known as ablation. It’s a relatively new treatment which is why not everyone is aware that it exists. That can make it difficult for a patient to make a fully-informed decision.”
Boers continues: “We need to carry on telling the world what we can offer. We’re making great progress, but are still at the pioneering stage. The professional association is campaigning for further training programmes, specific job profiles and a position within the hospital job structure. We’re gradually building on what we’ve achieved. As we see more and more examples of clinical technologists being successful at work, the added value we offer will become increasingly clear.”
[Update article]
The original article did not make it clear that the University of Twente has been offering a course for technical professions in the medical world since 2003. The Twente Director of Studies Heleen Miedema has worked hard for the BIG registration. Ineke Hoffschulte, former management director of the Faculty Club University of Twente, pointed this out to Delft Outlook in a letter to the editor (in Dutch).
Degree programme Clinical Technology
The six-year programme in Technical Medicine was designed by the University of Twente and started in 2003. The professional association NVvTG was founded in 2009 by technical physicians from Twente.
Following in the footsteps of the University of Twente, Leiden-Delft-Erasmus started the Bachelor of Clinical Technology in 2014 and the Master of Technical Medicine in 2017. The Clinical Technology program is a collaboration between Delft University of Technology (TU Delft), Leiden University (LUMC) and Erasmus University Rotterdam (Erasmus MC). These three centres already work together in the field of clinical-technological research in Medical Delta. Medical Delta is a collaboration platform that brings together the three renowned universities, two university medical centres, four colleges, governments, companies, healthcare institutions and other parties in South Holland and aims to use technological solutions to achieve sustainable care.